2017 Blog Entries
10/21/2017
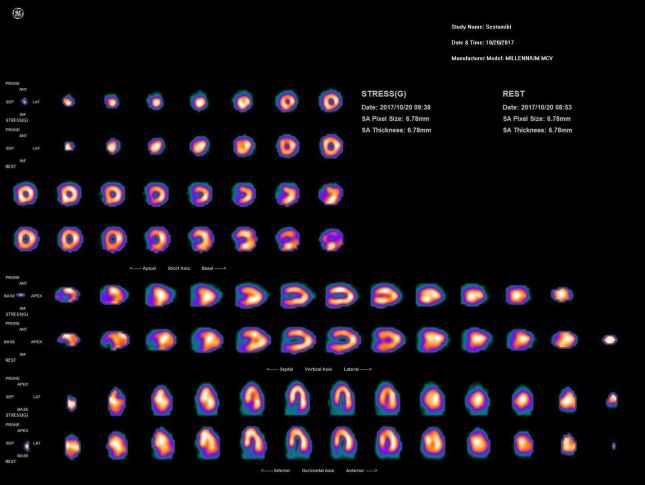
How do you manage your MPI patients that are severly claustrophobic without resorting to anxiolytics? At my main employer, we've instilled a novel, ultra-low
emission SPECT protocol (<6 seconds a stop if necessary) with both the rest and stress in a prone position. Having resolution recovery, like UltraSPECT, is what allows us
to lower the scan time while still preserving image quality as shown below.
This patients BMI is 39, imaged with a 7mCi (Rest), 21mCi (Stress) Sestamibi all-prone protocol on a GE MyoSight.
7/17/2017
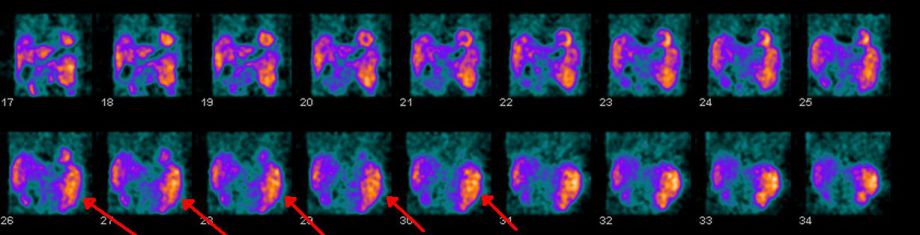
Here's a perfect example of how understanding a radiotracers normal/abnormal biodistribution can expedite a clinical diagnosis.
This patient had complaints of shortness of breath, and left upper quadrant pain.
Lets take a closer look at the rotating Tc99m-Sestamibi cine. It should be noted that the below raw images were acquired with lowered emission times using resolution recovery parameters.
Cardiac perfusion images were normal, however their spleen size was not, measuring 17cm on Ultrasound.
7/13/2017
Update: I've included a spread sheet making it easy to discern if the patient had a normal, intermediate, or blunted heart-rate response.
Is your Nuclear Cardiology Deparment documenting blunted heart rate responses? If not, this prognostic indicator, in addition to traditional MPI findings, adds a modest 15% improvement to the net reclassification (NRI).
As with Adenosine, when administering Regadenoson (Lexiscan) a normal increase in heart-rate will occur. A number of studies have shown that individuals whose
heart-rates don't respond, specifically anything <28%, was significantly associated with poor outcomes. These findings were with patients who had normal and abnormal
perfusion patterns.
Microsoft Excel sheet [10.8 KB]
6/21/2017
Out of all the technologies presented at this years annual SNMMI meeting, Ionetix raised the bar by displaying
it's miniature on-site cyclotron providing Nuclear Cardiology departments on-demand tracer production. This technology has the ability to address one of the biggest hurdles limiting the
propogation of Cardiac PET, that being a very sparse geographic network of industrial cyclotrons. Currently only N13-Ammonia is being offered (75mCi's every 10 minutes), but who knows what the
future holds with other positron emitters.
For those of you wanting more details on the technology, here's Ionetix's patent submission from 2011.
6/2/2017
Could this device eventually deliver a novel, preferred method of stress?
Image provided from Thornhillmedical.com
This SNMMI featured journal article is suggesting hypercapnic stimuli, when compared to Adenosine, could possibly be the new gold-standard for stress testing. Interesting to note that a contributing author Dr.Joseph Fisher, co-founder of Thornhill Medical, released in 2014 this paper, a conceptualized model proving CO2's vasodilatory effects on cerebral blood flow.
Adobe Acrobat document [3.1 MB]
Highlights from the article are as follows:
-MBF increased under hypercapnia and adenosine (P , 0.05, for all territories), albeit the increase in the LAD territory was significantly lower than in the LCx and RCA territories (with
hypercapnia and adenosine; both P , 0.05).
-Collective comparisons of regional MPR between hypercapnia and adenosine showed significant correlation (R 5 0.71, P , 0.05) and good agreement (bias 5 2.11%).
- There was a trend toward higher resting MBF before caffeine administration, but this was not statistically signifi- cant (P 5 0.09). However, the resting MBF normalized by rate–pressure product was
significantly higher before caffeine (1.5 · 1025 [preadministration] vs. 1.0 · 1025 [postadministration], P 5 0.03). These observations are consistent with reports in humans (22) and are likely
related to the influence of caffeine on calcium cycling at rest, which is known to promote vascular smooth muscle contraction (23,24).
-These findings of differential MBF response to hypercapnia and adenosine after the preadministration of caffeine suggest that the mechanism of action mediating myocardial hyperemia by these stimuli
are at least partly different.
-Found that when the PETCO2 is altered from rest (;35 mm Hg) to about 60 mm Hg under isoxic conditions, MBF increases to levels observed with the clinical dose of adenosine. Specifically, these
changes in MBF and MPR were both globally and regionally not different from those observed with adenosine in the absence and presence of coronary stenosis. Preadministration of caffeine abolished
myocardial hyperemia to adenosine, as expected, but not to hypercapnia.
-Hence our finding of marked increase in MBF under isoxic hypercapnia has significant translational value especially within the framework of cardiac stress testing. Because elevated levels of PaCO2
can introduce myocardial hyperemia to the same extent as adenosine, PaCO2 has the potential to be an alternative to these pharmacologic agents.
-The major side effect of hypercapnia is the psychic feeling of dyspnea.
-There are several advantages hypercapnia would provide over adenosine: it is noninvasive, it is inexpensive, and its onset is rapid (within 1 breath). As opposed to adenosine, its blood
concentration is known continuously from the end-exhaled concentration; its level is controlled within 2 mm Hg continuously throughout the test; the termination of a CO2 stimulus occurs within 10–15
s, as does its side effects; and there is no sudden severe headache, hypotension, tachycardia, diarrhea, allergy, or interaction with other drugs.
-As a further margin of safety, in the absence of hypoxia, there is no lethal level of PCO2.
Reason why A2A agonists won't be going away anytime soon:
-Notably, chronic obstructive pulmonary disease and CO2 retention would be a contraindication for a hypercapnic stimulus because they would not be able to mobilize the CO2 at the end of the test.
In these patients, an alternate stimulus such as adenosine would be needed.
5/30/2017
Privileged, and equally flattered, to be interviewed by BC Technical for a web-site case study.
5/19/17
For those of you in the Georgia region, the GSNMT annual meeting is taking place this weekend at the Atlanta
Marriott off 2000 Century Blvd. Going by what's on the agenda, it should be extremely informative!
Adobe Acrobat document [96.7 KB]
4/4/17
Back in January I posted a link to a JNM issue where Dr.Jeffry Siegel challenges the status quo on medical radiation:
Renowned Medical Physicist Jeffry A. Siegel
dispels the 70 year old hypothesis that exposure to medical radiation could increase ones risk of cancer. In fact, he suggests it more likely helps prevent it.
He emphasizes, "This fear is unjustified by any scientific findings and is discredited by most experimental and epidemiological studies, which show that low-dose radiation, instead, stimulates
protective responses provided by eons of evolution, resulting in beneficial effects."
Link to the JNM Issue can be found here.
Fast forward to the March 2017 JNM issue, and like ripples in a pond, numerous professionals
in the field are siding with Dr.Siegel. This issue alone has an astonishing five letters to the editor referencing his original article.
The concensus thus far weighs in favor of a complete overhaul which some argue "would
likely result in the elimination of many government jobs and significantly reduce the budget of the federal and state regulatory agencies." I for one am proud the JNM posted the controversial
article. It's a long overdue conversation with the NRC/BEIR
committee that
needs to happen sooner rather than later.
3/1/17
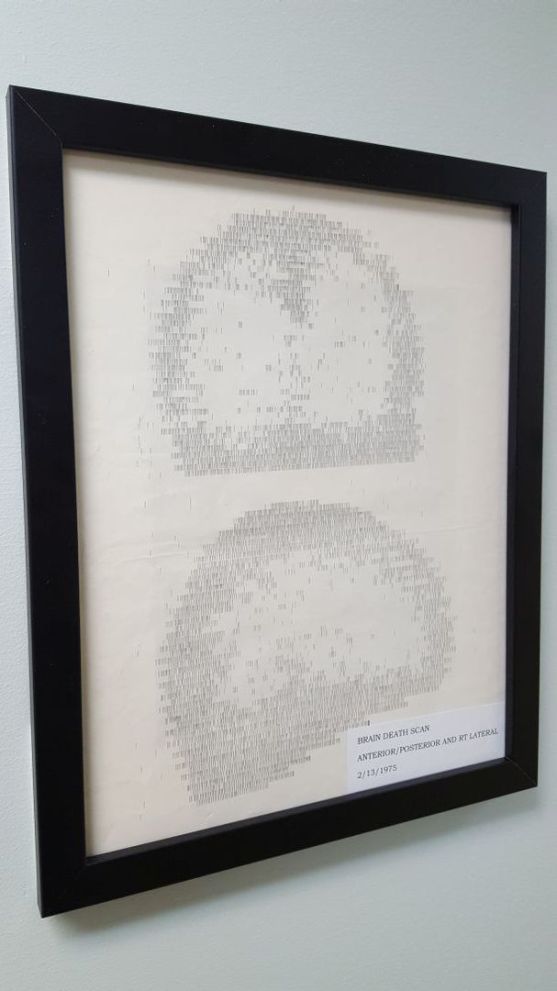
Just to show our patients how far Molecular Imaging has come, we've hung this cerebral pefusion scan from 1973 in our testing waiting room. The image was acquired via rectilinear scanner in 1973.
2/15/17
During the processing portion of myocardial perfusion imaging, most begin by first placing a region of interest
around the left ventricle. Next, the images are post-processed for quantitative analysis and reconstructed into short, horizontal, vertical sections. A question looms: How much time
was really spent analyzing the SPECT data for
normal/abnormal radiotracer biodistribution? Below is a Thallium-201 SPECT image acquired on a GE dual-headed Myosight. How much pathology can you find? *Answers below
Right Ventricular Uptake = Right ventricular overload from right-sided heart failure
Ascites = The liver isn't visualized. Should have hepatic/splencic radiotracer uptake. Findings may be from complications of right-sided heart
failure
Increased Lung-To-Left Ventricle Ratio = Indicative of left ventricular dysfunction
Lack of Renal Uptake = Normal functioning kidneys should have radiotracer uptake, renal disease/failure is indicated if not visualized
Thin Walled, Dilated Left Ventricle = Indicative of dilated cardiomyopathy
1/31/17
Dr.'s Siegel, Stabin, and Marcus take an unconventional jab at the NRC pleading they stop ignoring their
published work. Dr.Siegel specifically has been extremely vocal that current day medical radiation standards are based off unsubstantiated claims, guided by a 'radiophobic-centered,' not
scientific, approach.
Adobe Acrobat document [27.8 KB]
1/13/17
Is your Nuclear Cardiology Deparment documenting blunted heart rate responses? If not, this prognostic indicator, in addition to traditional MPI findings, adds
a 15% modest improvement to the net reclassification (NRI).
As with Adenosine, when administering Regadenoson (Lexiscan) a normal increase in heart-rate will occur. A number of studies have shown that individuals whose
heart-rates don't respond, specifically anything <28%, was significantly associated with poor outcomes. These findings were with patients who had normal and abnormal
perfusion patterns.
1/10/17
Renowned Medical Physicist Jeffry A. Siegel dispels the 70 year old hypothesis that exposure to medical radiation could increase ones risk of cancer. In fact, he suggests it more
likely helps prevent it.
He emphasizes, "This fear is unjustified by any scientific findings and is discredited by most experimental and epidemiological studies, which show that low-dose radiation, instead, stimulates
protective responses provided by eons of evolution, resulting in beneficial effects."
Link to the JNM Issue can be found here.
1/6/17
Will A2A agonists be the next big weight loss drug?
Adobe Acrobat document [3.4 MB]